
Andel Hoke suffered from lower back pain that was so painful she couldn’t sit at her desk. As an elementary school teacher, keeping up with her students was nearly impossible. Hoke tried daily to keep a positive attitude for her students. Outside the classroom each day, she began to isolate herself from family and friends.
“I couldn’t be my upbeat self,” she explains. The pain became so great that she was no longer able to participate in any activities with her students. Unsuccessful attempts to diagnose the source of her pain left her with no options and little hope. When standing or lying down became her only options, Hoke began losing her desire to live. “I didn’t want to bring the people I care about into my pain.”

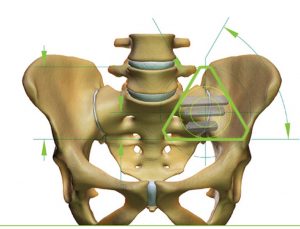
Her life took a positive turn when she met Dr. Andrew Manista at Olympia Orthopaedic Associates. When Dr. Manista heard Hoke’s story, he felt strongly that she was suffering from sacroiliac joint dysfunction. The sacroiliac joint, also known as the SI joint, is located between the sacrum and the pelvis. The SI joint plays a major role in reducing the impact of daily activities and provides support and stability. There are two joints located on either side of the body. It is an important shock absorber to prevent the impact of walking from reaching the spine. Hoke could not put any pressure on her spine without feeling incredible pain.
The damage to the SI joint is more common in women than in men. For many years this “forgotten joint” wasn’t even a consideration when diagnosing lower back pain. The pain often starts for women during pregnancy when the sacroiliac ligaments are loosened for childbirth. Patients who have undergone spine surgeries can develop problems post-surgery with their SI joint.
Dr. Manista admits that he wasn’t taught very much about this joint in medical school. The access point to the joint was so difficult and the surgery so unpleasant for the patient that it was rarely considered as a treatment option. When the iFuse Implant System was introduced, this all changed. Using the same technology used when repairing a fractured pelvis, the implant allows orthopedic surgeons to access the SI joint through a small incision.
“This surgery is a breakthrough for patients who have been suffering from undiagnosed lower back pain,” explains Dr. Manista. “Fifteen to twenty percent of patients with what we call failed back syndrome are actually suffering from SI joint dysfunction.”
Dr. Manista further explains, “Only about 10 percent of patients will need surgery.” Once the sacroiliac disease is diagnosed, many patients experience much less pain with physical therapy and proper pain management.
Dr. Manista was able to pinpoint the cause of Hoke’s pain by giving her an injection directly into the SI joint. “I literally melted on the table,” she says. The pain was gone and Dr. Manista knew that he had found the cause of her agony. The injection lasted about three weeks. Finally pain-free, Hoke was able to go to a movie and sit for the entire feature. She was the ideal surgical candidate for the SI Fuse implant.
The iFuse Implant System is a breakthrough treatment. The patented, triangular implant is designed to handle the stress of the sacrum, legs and spine all joining in one place. The titanium implant is coated with a patented plasma spray. The porous surface is designed to “grab” bone as it passes by. Bone will grow around the implant over time as the body heals and will strengthen the joint.

Dr. Manista performed the SI implant surgery on Hoke on a Friday morning and she was walking within an hour. “Today I can get on the floor and play with my students,” she says. “My whole outlook on life has changed now that I am pain-free.”
Dr. Manista now trains other surgeons from around the country on how to diagnose sacroiliac joint pain and implement the iFuse Implant System. Over 20,000 surgeries have been performed with the iFuse Implant System with a 90 percent success rate. Olympia Orthopaedics Associates has many non-surgical partners in the community. Cortisone injections, physical therapy and sacroiliac belts are all potential treatment options.
Drs. Douglas Taylor and Andrew Manista will be presenting an educational seminar on Sacroiliac Joint Pain at their Westside clinic on Thursday, February 16 from 6:00 p.m. – 7:00 p.m. For more information or to RSVP, please contact Rachel Sherburne at 360-570-4862.
Sponsored







































